Going Beyond Cholesterol
When most people have their cholesterol level checked they will usually have their ‘total cholesterol,’ LDL-C (the concentration of LDL), HDL-C (the concentration of HDL), triglycerides (TG), and non-HDL measured. However, while these measurements are of some use in estimating the risk of cardiovascular disease they do not give the full picture. More important than the mass concentration of the cholesterol-containing particles is the number of cholesterol particles and more besides.
When most people think about cholesterol they think that there is a good type and a bad type. In fact, all cholesterol is good. Cholesterol is vital to our existence. It is one of the most important constituents of our cell membranes. Not only do cell membranes provide structural support for the cell but they also facilitate how cells move, what goes in and out of cells and how cells interact with each other. Cholesterol is also essential in the production of steroid hormones, vitamins and bile acids which help digestion.
So cholesterol is good. It is only bad when it is in the wrong place and the wrong place for cholesterol to be is in the arterial wall. But how does cholesterol get there.
Only about a quarter of the cholesterol in our bodies comes from what we eat. The rest is produced by our bodies. Our liver manufactures about a fifth of the cholesterol made by our bodies. Of the cholesterol that we eat, most of it is not absorbed by our gut. So the amount of cholesterol that we eat only has a limited effect on the cholesterol levels in the body.
I think of the process of coronary artery disease as being a bit like my stag do in Bratislava. This may seem like a stretch, but bear with me. Think of the guys on the stag do as being like cholesterol particles. Just like the members of a drunken stag do in an unfamiliar town, cholesterol needs something to take it around the body. The things that help transport cholesterol around the body are called apoproteins. These are like the group of girls from a tour operator that the best man hires to take the stag do on a tour of the town’s bars. In the bloodstream, the cholesterol particles and apoproteins when packaged together are called apolipoproteins. These cholesterol particles with their apoprotein chaperones (aka apolipoproteins) all bundle together. The group of cholesterol particles and its apoprotein chaperone is called a lipoprotein.
Just like the group of girls from a stag-do tour operator, apoproteins help keep the group together and facilitate communication between the group and those outside the group. Apoproteins also help act as cofactors in enzyme reactions. This is akin to the female tour guides getting the stag group a round of free drinks when they arrive in a bar.
There are two important types of apolipoprotein – A and B. Apolipoprotein B (apoB) is almost always found with low-density lipoprotein (LDL). Think of low-density lipoprotein as a stag do with a female tour guide. Apolipoprotein A (apoA) is almost always found with high-density lipoprotein (HDL). Think of HDL as a tour group from a cruise ship with a nice tour guide. The are not going to cause trouble (unless the town is totally overrun with cruise ships and tour groups). An important point here, there is one ApoB molecule with one LDL particle. Each LDL particle is actually a group of cholesterol particles.
Most stag dos attract a few hangers-on. In the body, these unhelpful hangers-on are triglycerides. As the lipoproteins transport the cholesterol around the body these hangers-on drop away. Much the same happens on a stag do as it progresses.
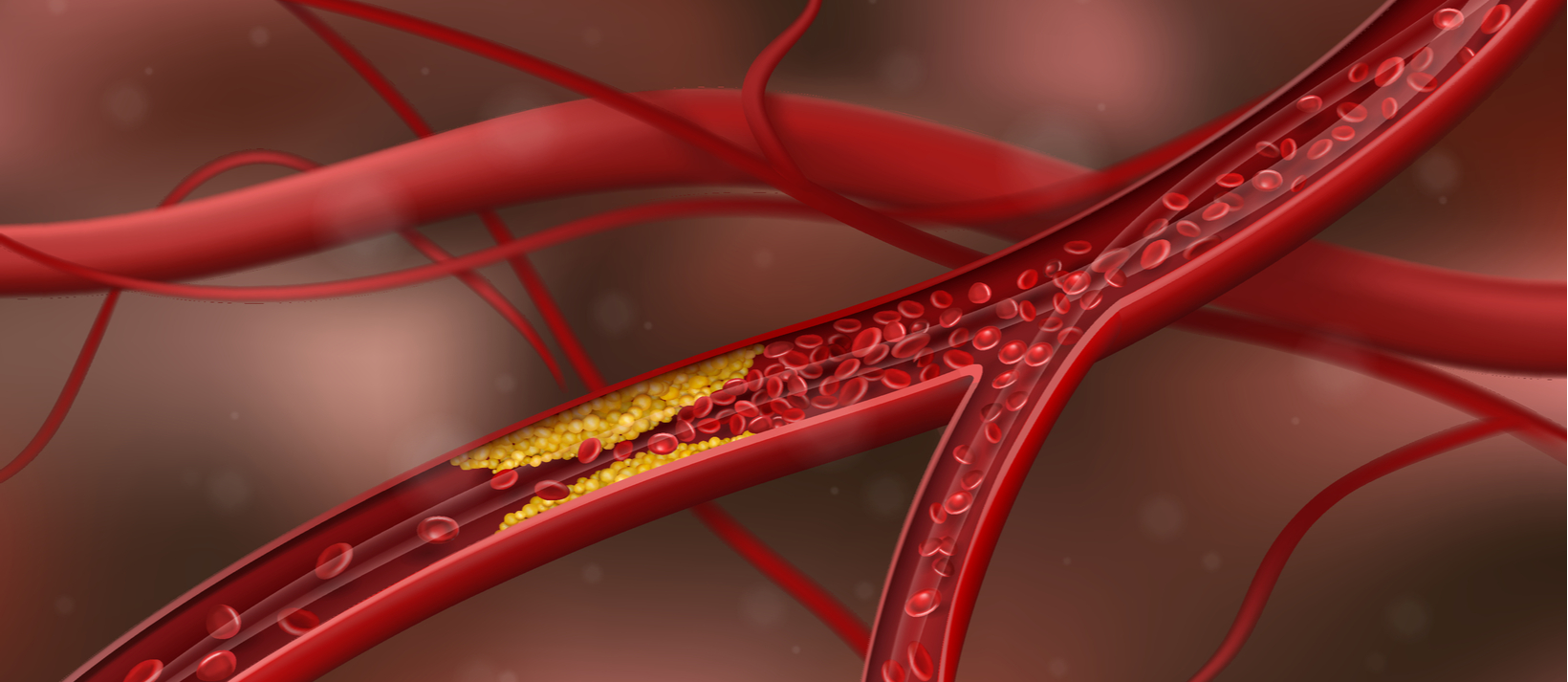
The lining of an artery is called the epithelium. To cause atherosclerosis, i.e. cardiovascular disease, the LDL particle has to enter the endothelium. If you can imagine the lining of the artery as being like a strip of nightclubs and bars and the lumen of the artery as being like a road. The stag do, of course, are the LDL particles. Apoprotein B can get the stag do into the cool club. Each stag do needs to have a girl with them to get in (because there is there is one ApoB molecule with one LDL particle). In the same way, to get into the lining of the arterial wall, each LDL particle needs an Apolipoprotein B to chaperone past the bouncer on the door. In case you’re wondering, the bouncer in this instance is called NPC1L1Niemann-Pick C1-Like 1 or NPC1L1 for short.
So what is it that causes LDL to go into the lining of the artery? Remember, conventional blood tests for cholesterol measure the concentration of the different lipoprotein subfractions. But, it is the number of particles of LDL that is more important. Think of it this way. The more small stag do groups there are the easier it is for each stag do to get into a bar. No bouncer is going to let a massive number of drunk guys in one big group into a bar. Bigger stag dos with more people in each of them are less likely to get into a bar. In the same way the higher the number of LDL particles the greater the chance they have of getting into the wall of the artery. Although LDL concentration may correspond to particle number, often it doesn’t.
Indeed, it has been found that the best predictor of the risk of cardiovascular disease is LDL particle number. Furthermore, those people at the highest risk had a low (normal) LDL-C and a high LDL particle number. In medical statistics, when two variables that usually track together do not track together, it is known as discordance. People who have high LDL-C and high LDL particle number are also at high risk but not as high as those with discordant values. Thinking about it in stag-do terms, the highest risk of trouble comes when lots of small stag dos are let into a bar. In the opposite scenario if there is just one stag do allowed in but it is large with lots of people who know each other the chance of trouble is low. That is, if there is a high LDL-C and low LDL particle number the risk of cardiovascular disease is actually less. As I have mentioned, having a large number of LDL particles and a high LDL-C is also a high risk for cardiovascular disease. It’s just not as high risk as having low LDL-C and high particle numbers. Even in patients who show up to the hospital having a heart attack, frequently their LDL-C is normal.
People with metabolic syndrome are more likely to have an unhelpful discordant relationship between LDL-C and LDL particle number. Metabolic syndrome is a condition in which people have raised triglycerides (a storage fat in the blood), raised blood pressure, elevated waist circumference and elevated blood sugar.
Once inside the club (the arterial lining) the stag do (LDL) causes all sorts of problems. Imagine members of the stag do hitting on local girls, being generally obnoxious and riling up groups of local guys. The same happens when LDL enters the endothelium – absolute pandemonium. This leads to inflammation in the arterial wall. On a stag do, the groups of locals might try to get rid of the stag do. But there are too many guys on the stag do. As you can imagine, the bar gets damaged. A brawl ensues and it spills out onto the street. Pretty much the same happens to the endothelium of the artery. The inflammatory response causes an arterial plaque to form which spills over into the lumen eventually causing a clot to form, blocking the artery. Think of the clot as the police being called. They then block off the street. This obviously means that bars and clubs further down the street have to close. This is equivalent to tissue ischaemia in our bodies where a lack of blood supply causes the tissues downstream to die. This is the process of a heart attack.
So although LDL-C can give us some information on the likelihood of having a heart attack, it is nowhere near as good as knowing the LDL particle number. Measuring this requires nuclear magnetic resonance spectrometry. This is very expensive. As there is one LDL per ApoB it turns out that ApoB is a good proxy for estimating LDL particle number and therefore cardiovascular risk. Indeed, several studies, including AMORIS, INTERHEART, IDEAL and the Leiden Heart Study have demonstrated that ApoB is superior in predicting cardiovascular disease risk. ApoB level is also useful in finding out how effective lifestyle changes and treatments have been. According to the INTERHEART and AMORIS trials, the best risk predictor of cardiovascular disease is the ratio between ApoB and ApoA1.
Ischaemic heart disease is, to a great extent, inflammatory. The real problem is not so much the presence of the LDL particle in the artery wall. It is the inflammatory response to the LDL that is the problem. LP-PLA is a marker of arterial inflammation and suggests that the formation of unstable plaques in the arteries is occurring. In our stag-do analogy, Lp-PLA is the equivalent of a group of bouncers entering the melee. It suggests that the arteries are angry and that arterial plaque is forming. The PLAC test measures the amount of lipoprotein-associated phospholipase (Lp-PLA2) in the blood. Lp-PLA is a key player in making plaques that line the arterial wall unstable and more likely to rupture.
Another way of estimating the amount of inflammation in our arteries is with hs-CRP. Other issues can cause a rise in hs-CRP. However, in a patient who is at high risk of cardiovascular disease, I associate high levels of hs-CRP with being at very high risk for cardiovascular disease.
So while traditional tests for cholesterol go some way to estimating cardiovascular risk, getting a much better estimation of risk requires a deep dive into different markers.
Dr J Hugh Coyne
Private GP
Parsons Green